Clinic for Gynecology with a Center for Oncological Surgery
Uterine fibroids are growths that form in the wall of the uterus. There is practically no degeneration, i.e. the fibroids becoming malignant. In the vast majority of cases, fibroids are benign in nature, which means that they cannot metastasize or spread. They are often, often completely asymptomatic. In women between 40 and 50, such tumors are detectable in over 50% of the ultrasound examination.
Fibroids arise and grow under the influence of female sex hormones, which are mainly produced in the ovaries. Hereditary factors are probably also responsible for the development of fibroids. Fibroids can grow quickly or slowly, continuously or intermittently.
Myoma-related symptoms practically always disappear after the menopause when the estrogen level (estrogen is a female sex hormone) falls and the fibroids shrink.
However, if women now undergo hormone (replacement) therapy during or after the menopause, the shrinkage does not occur and there may even be growth, so that the myoma-related symptoms persist.
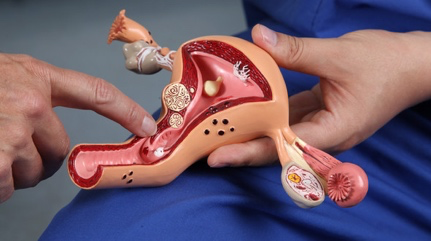
Different types of fibroids:
- submucous fibroids: located in the uterine cavity just below the lining of the uterus;
- intramural fibroids: located in the wall of the uterus;
- Subserous fibroids: are located on the outside of the surface of the uterus.
Uterine fibroids are often asymptomatic, but depending on their size, location and number, they can cause both mild and severe symptoms. The submucous fibroids cause bleeding disorders even when they are small, especially increased bleeding. Myomas in the uterine wall tend to cause painful menstrual bleeding. Fibroids on the surface can grow for a long time without causing discomfort until they become noticeable through pressure on the neighboring organs.
Women with fibroids report one or more of the following symptoms:
- increased and prolonged menstrual bleeding, sometimes with clotting (clotted blood);
- Abdominal pain;
- Pressure, foreign body, or heaviness in the pelvic area;
- Pain in the back or radiating into the legs;
- Painful intercourse;
- Feeling of pressure on the bladder with increased urge to urinate;
- Feelings of pressure on the intestines, possibly associated with pain and gas;
- rare: greatly enlarged waist circumference.
1. Consultation hour: diagnostics and therapy planning
Larger fibroids can be felt during the pelvic examination. During the ultrasound examination, smaller fibroids can be seen. If the findings are unclear, a hysteroscopy or a laparoscopy (laparoscopy / pelviscopy) can help. The fibroids can also be removed.
At the Charité, we offer you the full range of modern diagnostic and treatment methods. Fibroids that do not cause symptoms usually do not need to be treated. However, if a desired pregnancy does not occur or if miscarriages are caused by myomas, removal is advisable. Likewise with bleeding disorders or pain and with unchecked growth in size. Removal is almost always possible using minimally invasive surgical techniques (laparoscopy or uteroscopy). The uterus can be preserved. If there are large and numerous fibroids and / or if there is no desire to have children, removal of the uterus can be useful.
Myoma therapy often begins with an attempt to treat medication, e.g. with a special birth control pill or other temporary hormone or hormone receptor therapy. If this course of treatment is not possible or unsuccessful, direct treatment or removal of the fibroids should be planned. In principle, this can be done in two ways — by non-invasive or less invasive radiological procedures or by so-called minimally invasive surgical gynecological procedures. Each of the procedures has advantages, but also disadvantages and side effects. Not every treatment method is equally suitable for every patient.
First of all, your gynecologist will advise you. With a corresponding referral, we can then discuss in our clinic myoma consultation which procedure is best for you. We advise you in the myoma consultation hour of the Berlin Charité on the Virchow-Klinikum campus individually, comprehensively and openly about both uterus-preserving (i.e. no uterine removal) surgical procedures and non-gynecological myoma therapy procedures.
In addition to your wishes, the size, position and number of the fibroid nodes that are present are decisive for the decision. In addition, the decision-making should include whether you still want to have children and whether you, in principle, want the uterus to be preserved regardless of this.
We are happy to advise you and also offer you the various treatment methods in the clinic.
With every operation and every non-surgical treatment measure, including a benign finding, you should weigh the risks and complications of the procedure against the advantages and the (expected) gain in quality of life. We always recommend getting a competent second opinion, at least before a major operation.
Fibroids and pregnancy
In principle, pregnancy is also possible with a fibroid, especially if the fibroid is small and / or on the outside of the uterus.
Various factors, both on the male and female part, can prevent pregnancy from occurring. If the man has been shown to be fertile and there are no other medical reasons for a couple to be infertile, changes in the uterus may be the cause. At least those fibroids that narrow the interior of the uterus, in which the fertilized egg is implanted and the embryo grows, should be treated.
With every therapy method, operative or non-operative, the treatment risks must be weighed against the expected improvements in the situation for pregnancy. After fibroid surgery, we recommend not becoming pregnant for about three months. After that, pregnancy should be possible.
2. Operative therapies
Fibroid peeling
Fibroid peeling is a surgical procedure in which only the fibroids are removed and the uterus is preserved. There are different ways to peel the fibroid out, depending on the location, size and number of the fibroid nodes, the way via the vagina (hysteroscopic), a laparoscopy (laparoscopic) or an abdominal incision is chosen. All interventions are usually carried out under general anesthesia and require a stay of several days in the clinic after the operation.
Hysterectomy
The removal of the entire uterus (with or without the cervix; the ovaries remain in the body in any case) can, depending on the size of the organ, through the vagina, laparoscopy, combined laparoscopy and through the vagina or, in the case of a very large uterus, also through an abdominal incision can be performed. If family planning has been completed, severe myoma-related symptoms and the desire to definitely avoid bleeding, a hysterectomy is a good treatment option. It is usually performed under general anesthesia and involves a 3 to 7 day hospital stay. Pregnancy is no longer possible after the uterus has been removed.
3. Non-operative therapies
In the last 10 to 15 years, two methods have become established that are carried out by radiologists.
Uterine fibroid embolization
This treatment is carried out by a specialized radiologist. After a local anesthetic in the groin area, a small plastic tube is inserted painlessly to the uterine artery via an access similar to that used for a blood sample under X‑ray control (fluoroscopy). Through this, small plastic or gelatin beads the size of grains of sand are injected into the small arteries that supply the uterine fibroids with blood. This will cut them off from the bloodstream and the fibroids will shrink by up to 50% within a few months of the procedure.
Uterine artery embolization alone is now an established method for myoma therapy as an alternative to surgery worldwide. A direct combination of embolization with a myoma operation one or two days later can be useful when it comes to preserving the uterus, even though it is very much enlarged by one or more myoma nodes (up to or even over Navel height).
In these cases, an operation is often difficult and can be associated with very heavy bleeding, which can be significantly reduced with the embolization carried out (a few days before the operation). This increases the chances of preserving the uterus.
MRI-guided focused ultrasound
The second method is MRI-guided focused ultrasound, which can reduce the size of the fibroids by up to 30–40%. Here you lie in a tubular magnetic resonance tomograph (MRI). This takes pictures of your uterus with the fibroid. Das Verfahren basiert auf einem starken Magnetfeld und der Einstrahlung von Radiowellen, für die der Mensch nicht empfindlich ist. With the help of the recordings, ultrasound waves are aimed at your fibroid by a radiologist and the fibroid is reduced in size in several portions by the heat generated. You do not feel any pain.
4. Follow-up care
In principle, with all uterine-preserving treatment measures, both operative and non-operative, there is a possibility that myomas will develop again after a few years. As part of your routine checkups, you should address any recurring symptoms or new symptoms.